UP TO DATE INFORMATION AND NEWS RELATED TO CANCER RESEARCH AND TREATMENT FOR CANCER PATIENTS AND COMMUNITY.
TRANSLATE
Sunday, 31 December 2017
Thursday, 28 December 2017
Watch this 6-minutes interesting video about breast cancer sign, symptoms and risk factors.
https://www.youtube.com/watch?v=Jv4K4InGvDw&feature=youtu.be#cancer #breast cancer #CancerHelpOnlin #research #breast #oncology
Wednesday, 27 December 2017
Scientists have developed a DNA test that diagnoses deadly breast cancer one year earlier than current methods
- Changes in a part of DNA, known as EFC#93, are an early warning sign
- These changes occur in patients' blood before cancer becomes detectable
- Among women with these changes, 43% were diagnosed in 3-6 months
- Some 25% of women with EFC#93 in their blood were diagnosed in 6-12 months
- The test's accuracy may avoid unnecessary treatment in less severe cases
Scientists have developed a DNA test that may diagnose fatal breast cancer year
earlier than current methods.
Changes in a part of DNA, which the researchers named EFC#93, suggests early warning signs of life-threatening breast cancer.
These changes occur in patients' blood before their cancer becomes detectable in their breast tissue.
A study revealed among women who have EFC#93 in their blood, 43 per cent were diagnosed with a life-threatening form of breast cancer three-to-six months later, while 25 per cent were diagnosed within six-to-12 months.
Study author Professor Martin Widschwendter from University College London, said: 'For the first time, our study provides evidence that markers such as EFC#93 provide a highly specific indicator that could diagnose fatal breast cancers up to one year in advance of current diagnosis.'
'This may enable individualised treatment, which could even begin in the absence of radiological evidence in the breast.'
There are around 55,000 new cases of breast cancer every year in the UK, with one in eight women being affected at some point in their lives.
Changes in a part of DNA, which the researchers named EFC#93, suggests early warning signs of life-threatening breast cancer.
These changes occur in patients' blood before their cancer becomes detectable in their breast tissue.
A study revealed among women who have EFC#93 in their blood, 43 per cent were diagnosed with a life-threatening form of breast cancer three-to-six months later, while 25 per cent were diagnosed within six-to-12 months.
Study author Professor Martin Widschwendter from University College London, said: 'For the first time, our study provides evidence that markers such as EFC#93 provide a highly specific indicator that could diagnose fatal breast cancers up to one year in advance of current diagnosis.'
'This may enable individualised treatment, which could even begin in the absence of radiological evidence in the breast.'
There are around 55,000 new cases of breast cancer every year in the UK, with one in eight women being affected at some point in their lives.
Tuesday, 19 December 2017
Sentinel lymph node biopsy for breast cancer
What is a sentinel lymph node?
A sentinel lymph node is defined as the first lymph node to which cancer cells are most likely to spread from a primsry tumor. Sometimes, there can be more than one sentinel lymph node.
What is a sentinel lymph node biopsy?
A sentinel lymph node biopsy (SLNB) is a procedure in which the sentinel lymph node is identified, removed, and examined to determine whether cancer cells are present.
A negative SLNB result suggests that cancer has not developed the ability to spread to nearby lymph nodes or other organs. A positive SLNB result indicates that cancer is present in the sentinel lymph node and may be present in other nearby lymph nodes (called regional lymph nodes) and, possibly, other organs. This information can help a doctor determine the stage of the cancer (extent of the disease within the body) and develop an appropriate treatment plan.
A negative SLNB result suggests that cancer has not developed the ability to spread to nearby lymph nodes or other organs. A positive SLNB result indicates that cancer is present in the sentinel lymph node and may be present in other nearby lymph nodes (called regional lymph nodes) and, possibly, other organs. This information can help a doctor determine the stage of the cancer (extent of the disease within the body) and develop an appropriate treatment plan.
What happens during an SLNB?
A surgeon injects a radioactive substance, a blue dye, or both near the tumor to locate the position of the sentinel lymph node. The surgeon then uses a device that detects radioactivity to find the sentinel node or looks for lymph nodes that are stained with the blue dye. Once the sentinel lymph node is located, the surgeon makes a small incision (about 1/2 inch) in the overlying skin and removes the node.
 |
The sentinel node is then checked for the presence of cancer cells by a pathologist. If cancer is found, the surgeon may remove additional lymph nodes, either during the same biopsy procedure or during a follow-up surgical procedure. SLNBs may be done on an outpatient basis or may require a short stay in the hospital.
SLNB is usually done at the same time the primary tumor is removed. However, the procedure can also be done either before or after removal of the tumor.
What are the benefits of SLNB?
In addition to helping doctors stage cancers and estimate the risk that tumor cells have developed the ability to spread to other parts of the body, SLNB may help some patients avoid more extensive lymph node surgery. Removing additional nearby lymph nodes to look for cancer cells may not be necessary if the sentinel node is negative for cancer. All lymph node surgery can have adverse effects, and some of these effects may be reduced or avoided if fewer lymph nodes are removed like lympheedema, seroma, numbness qand difficulty to move the arm.
Tuesday, 12 December 2017
What is the abscopal effect?
In oncology, the
abscopal effect refers to the ability of localized radiation to trigger
systemic antitumor effects and achieve a systemic tumor response. The abscopal
effect has been demostrated in mouse model and observed in human as well. The abscopal mechanism has been elucidated by
the work of many investigators who showed that this process was likely mediated
by the immune system leading to immunogenic tumor cell death, a process that
involves dendritic cells, T regulatory cells, and suppressor cells as critical
mediators. The recent successes of several immune checkpoint inhibitor clinical
trials in various malignancies have demonstrated wide applicability and
enormous therapeutic potential of immunomodulation and have galvanized keen
interest in this field. An ambitious goal of combining radiotherapy and
immunotherapy in the clinic would be long-term remission for cancer patients
with metastatic disease, perhaps through an approach analogous to delivering an
in-situ anti-tumor vaccine.
Find below a cartoon
showing the abscopal effect in mouse model where a distant tumor lesion on the
right flank disappears after treating with local radiation therapy another
distant tumor lesion on the left flank.
Monday, 11 December 2017
Most frequent mamography findings at glance
Mammograms are pictures (x-rays) of the breast, used to check for breast cancer. Possible mammogram findings include:
- Lumps (mass or tumor). Lumps come in different sizes and shapes. Fluid-filled cystics are usually smooth and rounded, with clear, defined edges and are not cancer. Lumps that have a jagged outline and an irregular shape are of more concern.
- Calcifications. There are two types of breast calcifications, or calcium deposits:
- Macrocalcifications which look like small white dots on a mammogram. They are often caused by aging, an old injury, or inflammation and are usually bening.
- Microcalcifications, which look like white specks on a mammogram. If found in an area of rapidly dividing cells or grouped together in a certain way, they may be a sign of DCIS or breast cancer.
- Dense breat tissue: A dense breast has relatively less fat and more glandular and connective tissue. This mammogram finding is both common and normal, especially among younger women and women who use menospuasal hormone therapy. Dense breast tissue can make a mammogram more difficult to interpret because both dense breast tissue and breast tumors appear as solid white areas in the image.
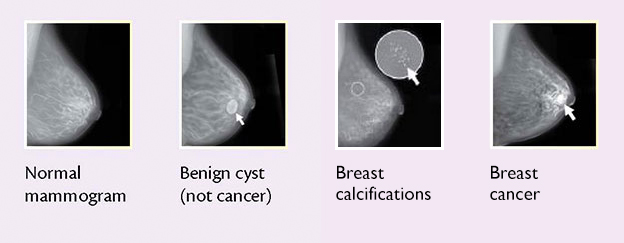 |
| Pictures with different findings on the mammograms |
Where the name of cesarean section is coming from?
The early history of cesarean
section remains shrouded in myth and is of dubious accuracy. Even the origin of
"cesarean" has apparently been distorted over time. It is commonly
believed to be derived from the surgical birth of Julius Caesar, however this seems
unlikely since his mother Aurelia is reputed to have lived to hear of her son's
invasion of Britain. At that time the procedure was performed only when the
mother was dead or dying, as an attempt to save the child for a state wishing
to increase its population. Roman law under Caesar decreed that all women who
were so fated by childbirth must be cut open; hence, cesarean. Other possible
Latin origins include the verb "caedare," meaning to cut, and the
term "caesones" that was applied to infants born by postmortem
operations. Ultimately, though, we cannot be sure of where or when the term cesarean was derived. Until the sixteenth and
seventeenth centuries the procedure was known as cesarean operation. This began
to change following the publication in 1598 of Jacques Guillimeau's book on
midwifery in which he introduced the term "section." Increasingly
thereafter "section" replaced "operation."
One of the earliest
printed illustrations of Cesarean section. Purportedly the birth of Julius
Caesar. A live infant being surgically removed from a dead woman. From
Suetonius' Lives
of the Twelve Caesars, 1506 woodcut.
Subscribe to:
Comments (Atom)







